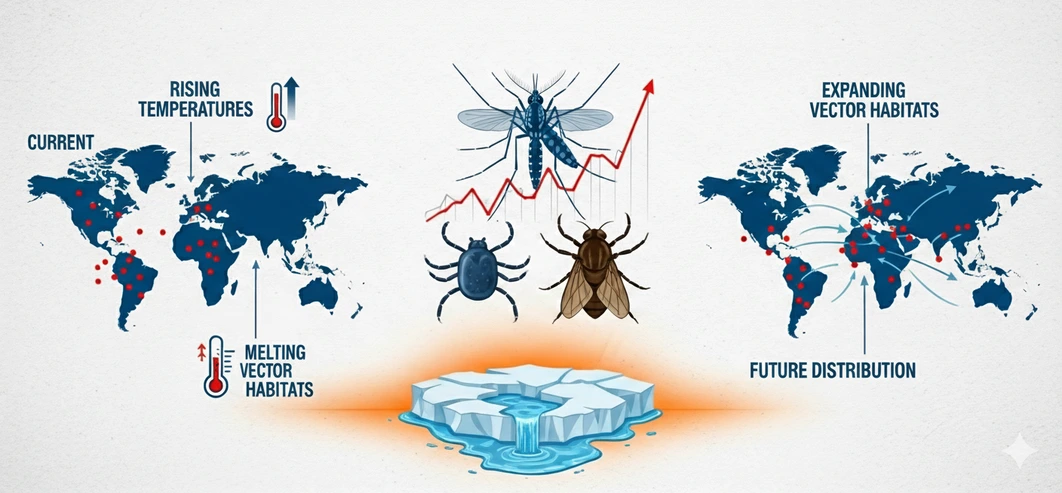
New Delhi / Global – In 2025, the connection between climate change and public health is undeniable. As global temperatures increase, the threat of diseases transmitted by dengue, malaria, chikungunya and zika – is intensifying vectors. These diseases, once limited to tropical zones, are now expanding to seasoned climates such as southern Europe, South America and high altitude regions in southern Asia. The heated planet is changing disease patterns – and the world must respond.
Hot Climates and the Rise of Vector-Borne Diseases
Climate change is transforming mosquito ecology, primary dengue and malaria vectors. Increasing temperatures, increased rainfall and higher humidity create perfect reproduction conditions. In addition, the warmer climate speeds up mosquito life cycles and reduces the period of viral incubation, making disease transmission faster and more widespread.
According to the World Health Organization (2023), climate change is now an important factor behind the overall increase in vector – transmitted infections. In 2025, countries such as Nepal, northern India and parts of Europe – previously very cool for mosquitoes – are now reporting seasonal outbreaks of dengue.
Climate – Driven Disease Resurgence in 2025
In the last two decades, global health systems have made substantial progress in malaria control. However, in 2025, new climate -oriented standards are reversing this trend. Unpredictable rains create stagnant water bodies, ideal for Anopheles mosquitoes, which spread malaria. At the same time, dengue cases exploded – especially in Urban Asia, where more than 500 million people are at risk.
The Lancet Countdown 2024 report found that since 2000, the adequacy of the climate for dengue has increased by 18% worldwide, with the most sharp growth in low and medium -income countries. These areas are usually the least equipped to respond effectively.
Are Health Systems Ready for Vector-Borne Diseases?
Despite the initial warnings, most countries remain poorly prepared. Public health infrastructure lacks in many regions :
- Climate – integrated disease surveillance
- Trained vector control staff
- Predictive weather – health models
As a result, outbreaks are usually detected too late. Meanwhile, rapid urbanization, poor sanitation and inadequate housing continue to expose vulnerable populations, including the elderly, children and people in low – income communities.
Necessary Public Health Actions in a World of Heating
To respond to the growing threat of climate disease – linked, global and local health systems must adopt climate informed strategies, such as :
- Integration of early warning systems in disease monitoring
- Expanding community – based vector control programs
- Invest in vaccination efforts (e.g. new dengue vaccines)
- Improving international coordination and data sharing
The IPCC AR6 Report (2022) warns that, without urgent adaptation, public health risks related to climate change will only increase. The time to act is now.
Conclusion – A Climate – Health Emergency in Motion
In 2025, vectors – transmitted diseases serve as public health emergencies and climate change indicators. The resurgence of malaria and dengue in new territories highlights the need for :
- Stronger health systems
- Integrated climate and health policies
- Global solidarity in disease response
Finally, the future of public health depends on how decisively we face climate change today. By adapting our strategies, investing in resilience and protecting the most vulnerable, we can turn the tide.


